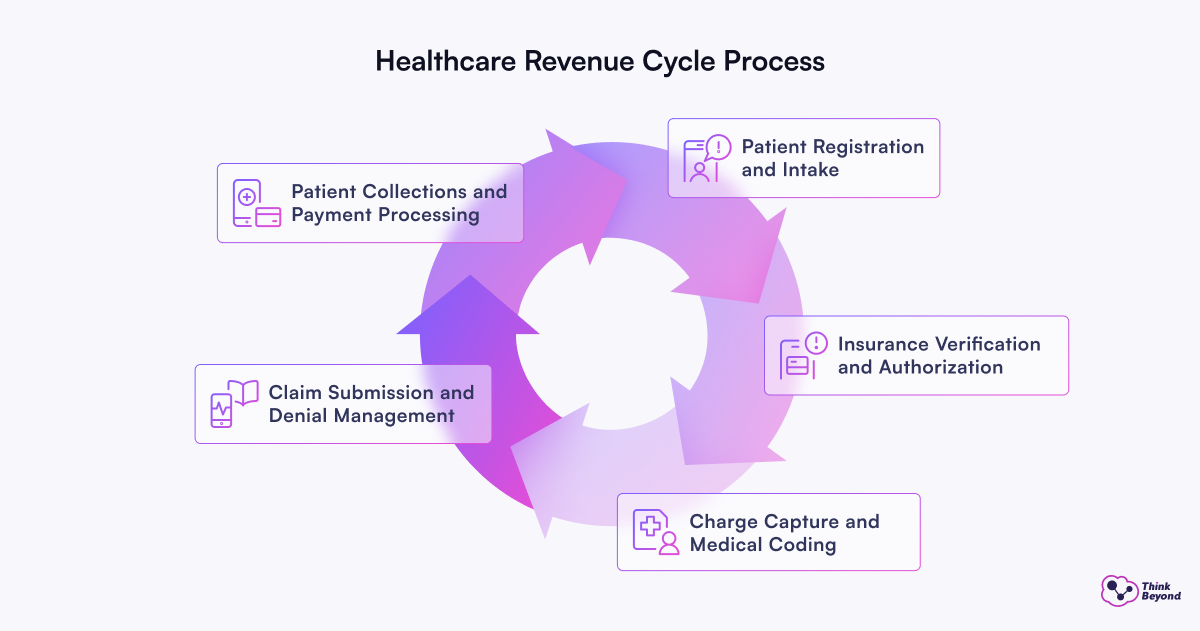
Healthcare’s revenue lifecycle management involves six important stages. These stages start with patient registration and insurance checks. The process continues until final payment and analysis. Many healthcare providers don’t deal very well with inefficiencies. A single invoice takes 12 minutes to create. This time adds up quickly as patient numbers increase.
Salesforce tackles these issues through integrated solutions like Revenue Cloud. This reliable system uses automation and evidence-based insights to streamline the entire revenue lifecycle. But it does more than simple financial management. It combines revenue and CRM processes into one system. This gives healthcare organizations complete control over revenue growth while meeting regulatory requirements.
What is the Healthcare Revenue Cycle and Why Does It Matter?
The healthcare revenue cycle tracks patient care from registration to final payment through a series of financial and administrative processes. Healthcare organizations need to pay close attention to each stage to maximize reimbursements.
1. Patient Registration and Intake
Patient registration kicks off the revenue cycle and includes collecting demographic, social, clinical data, and insurance information. This first step builds the foundation for all billing activities that follow. Research shows that more than half of claim denials come from mistakes made at the start. The process needs to work better. Many outpatient facilities still ask patients to fill out the same paperwork at every visit, whatever their gender, age, or reason for visiting. Digital patient intake solutions help providers make these processes smoother. Staff members can focus on patient care instead of paperwork.
2. Insurance Verification and Authorization
Staff members contact insurance carriers to check eligibility, insurance limits, co-pays, deductibles, and exclusions. Some procedures need pre-authorization, which means providers must get approval from the patient’s insurance payer first. This step will give a clear picture that services meet medical requirements and prevent future claim denials.
3. Charge Capture and Medical Coding
Charge capture tracks all billable services given to patients, from procedures to treatments and supplies. Medical coding turns these healthcare services into standard codes using systems like ICD-10 for diagnoses and CPT for procedures. A hospital can lose millions in revenue due to missed charges. Medical coders study patient documentation to pick the right codes that show medical necessity and care complexity.
4. Claim Submission and Denial Management
Claims go to payers for reimbursement after coding. In spite of that, denials have grown by 20% across the industry in the past five years. Good denial management looks at why claims get denied, appeals when needed, and stops future denials from happening.
5. Patient Collections and Payment Processing
The final stage bills patients for balances left after insurance processing. Studies show 96% of patients want to know costs upfront, but 64% don’t get this information. On top of that, 60% of patients prefer to pay online, which shows the need for digital billing options. Payment tools help staff focus on high-value accounts based on patients’ ability and likelihood to pay. This helps collect more money with fewer resources.
Top Challenges Healthcare Providers Face in Revenue Management
Healthcare providers lose a lot of money due to administrative errors in revenue management. The quality of patient care suffers as organizations try to handle complex billing systems that threaten their stability.
- Medical coding creates major hurdles for healthcare organizations. Each payer has its own rules and policies for medical coding and billing that keep changing.
- Healthcare organizations take direct financial hits from credentialing delays. Providers must wait 90–120 days on average before they can bill for their services, even though they keep seeing patients.
- Patient safety suffers when information gets scattered across departments or systems. Information gets stuck in specific departments, healthcare facilities, or individual electronic health record systems, creating data silos.
- A Ponemon Institute survey shows that regular HIPAA training helps organizations avoid data breaches. Healthcare organizations must balance strong data security with their use of analytics tools.
- Live analytics help administrators track financial performance and spot trends to make evidence-based decisions. These tools also help manage denials by identifying patterns in rejected claims. Staff can then be trained to resolve common problems.
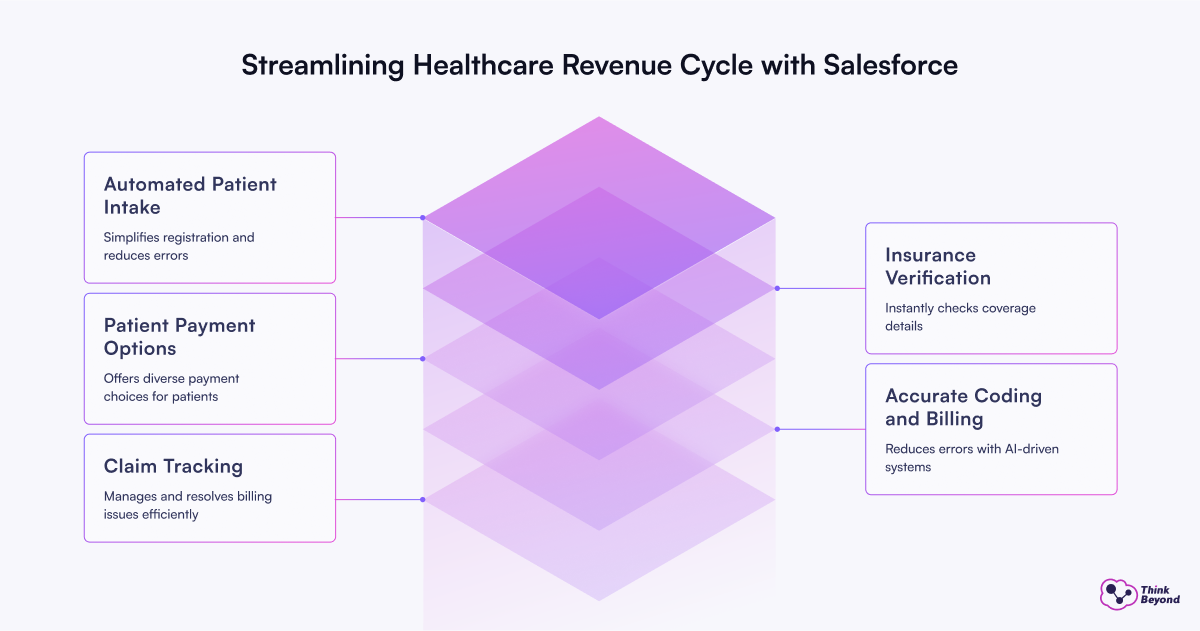
How Salesforce Streamlines Each Stage of the Revenue Cycle
Salesforce gives healthcare providers specialized tools that solve critical problems throughout the revenue cycle. Their cloud solutions help providers replace scattered manual processes with simplified digital ones.
Automated Patient Intake with Salesforce Health Cloud
Health Cloud unites patient data from all sizes of operations, while it automates registration. This reduces errors that often happen during manual data entry. The platform lets patients register online quickly and validates data instantly while updating their records automatically. Patient profiles in Health Cloud bring together information from many sources and eliminate data silos that often slow down billing.
Up-to-the-minute Insurance Verification via MuleSoft Integration
MuleSoft Accelerator for Healthcare lets staff check benefits instantly within the Salesforce Health Cloud. Staff members can now check a patient’s insurance coverage electronically without jumping between systems. The Benefits Verification API pulls coverage details from major eligibility providers into Health Cloud, making verification instant rather than relying on phone or fax.
Accurate Coding and Billing with Contracts AI
Agentforce by Salesforce checks claims instantly and flags risky submissions to alert billing teams about possible issues. This proactive fraud detection protects revenue while keeping the claims process transparent. AI-driven coding systems cut billing errors by up to 40% by automating data extraction and classification.
Claim Tracking and Denial Management in Service Cloud
Service Cloud’s case management features speed up billing issue resolution and improve cash flow. Case objects in Health Cloud combine every patient interaction into single data points. The system then routes each case to team members based on their skills, workload, and priorities. This setup helps catch missing information, duplicate claims, and coverage details that might cause denials.
Patient Payment Gateways and Self-Service Tools
Salesforce helps healthcare providers give patients several payment choices:
- Credit cards and debit cards
- Digital wallets
- Scheduled automated payments
These payment options, combined with Salesforce integration, cut payment processing costs. Up-to-the-minute data analysis and reporting tools help administrators track payment patterns and outstanding balances. Automated payment processing reduces manual data entry needs and saves valuable time for administrative staff.
The Future of Revenue Management: Subscription-Based Healthcare
Healthcare providers now turn to subscription models to create steady revenue streams. These models offer reliable income and make patients happier by giving them better access to care, unlike the traditional pay-per-service approach.
Healthcare Subscriptions as a Revenue Model in the U.S.
Subscription-based healthcare continues to grow across the United States. The subscription e-commerce market has shown annual revenue growth rates exceeding 100%. Direct Primary Care (DPC) shows this trend well. Patients pay monthly fees between USD 25.00 and USD 100.00 to access primary care services. This “Netflix-like” subscription model works well in the United Kingdom, Australia, and Sweden. Traditional reimbursement systems don’t deal very well with innovation, but this model fixes those limitations.
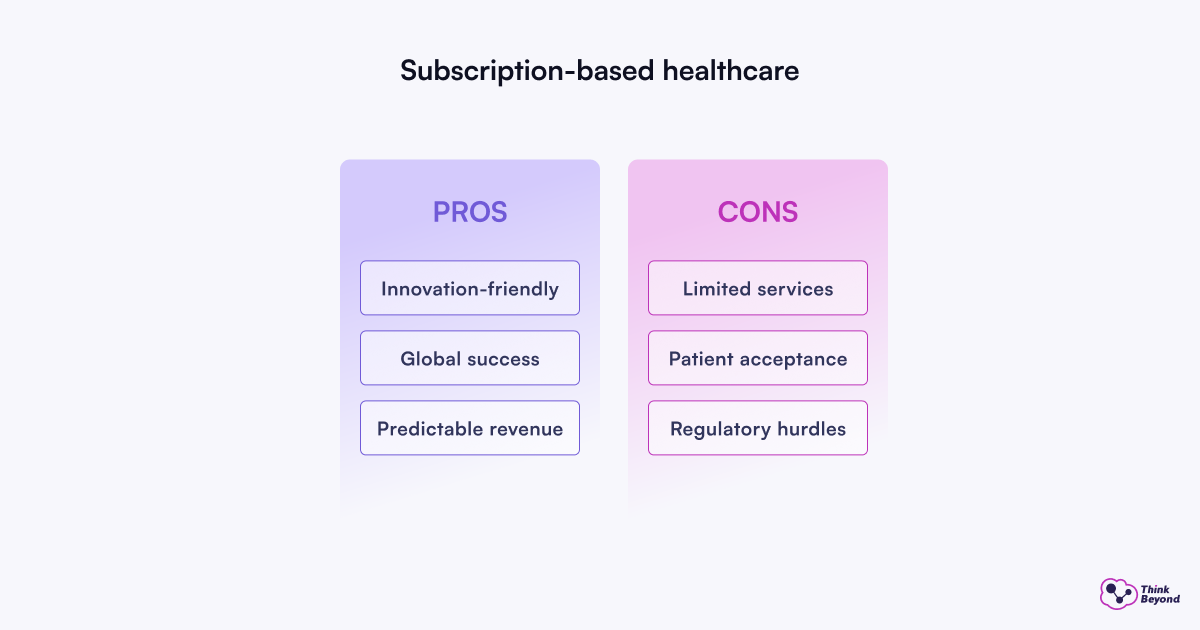
Salesforce Support for Subscription Billing Models
Salesforce Revenue Cloud offers detailed tools to manage healthcare subscriptions. The platform takes care of recurring services, usage-based pricing, and automatic renewals. It creates contracts, invoices, and payment schedules while automating every step. Healthcare organizations with specific billing needs can stay accurate and follow regulations.
Linking Subscription Models to Revenue Cloud Salesforce
Revenue Cloud combines smoothly with payment gateways for PCI-compliant credit card and ACH transactions (USA). Organizations using Salesforce solutions see an increase in forecast accuracy, more upsells and cross-sells, and better pricing compliance. On top of that, it offers flexible payment terms with time-based, usage-based, and milestone-based billing plans that suit patient needs better.
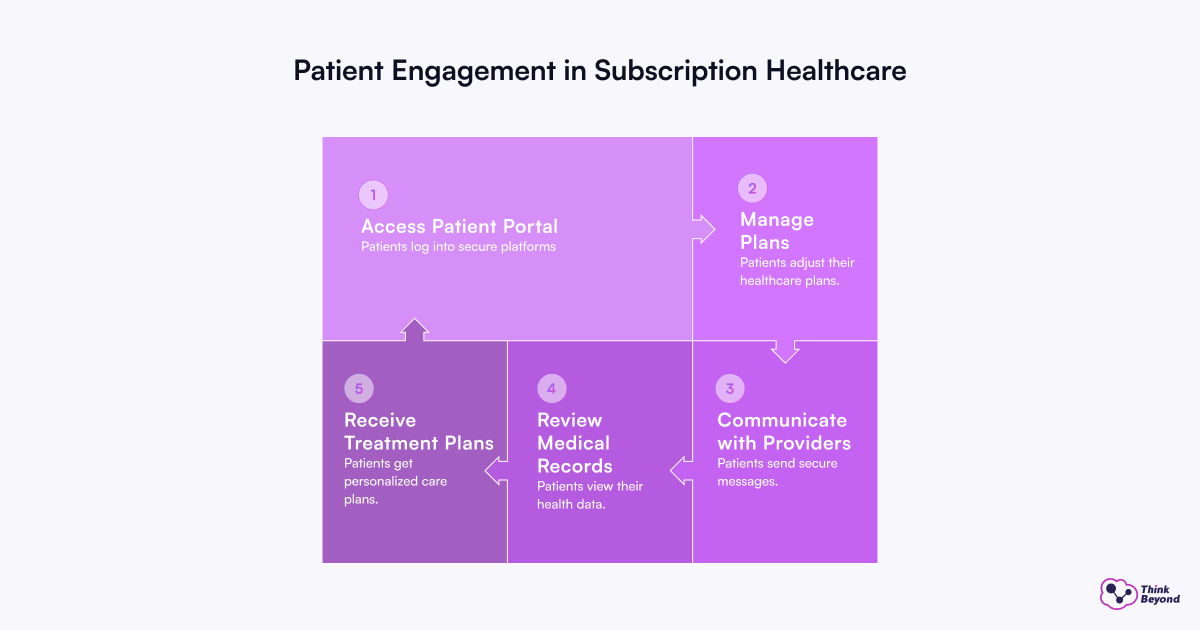
Patient Engagement in Subscription Healthcare Plans
Patient portals, based on Experience Cloud, make subscription-based healthcare more convenient and available. These secure, HIPAA-compliant platforms let members:
- Change or upgrade their plans when needed
- Send secure messages to their providers
- See their medical records, lab results, and individual-specific treatment plans
Subscription healthcare gives providers steady, predictable income while offering clear, affordable care to patients.
Smart Revenue for Healthcare, Built on Salesforce
The goal of Salesforce for Revenue Cycle Management (RCM) in the healthcare industry is to provide a smooth, patient-focused financial experience that supports the provision of high-quality care, not just to get paid. Healthcare providers:
- Gain a comprehensive view of their revenue cycle from patient intake to final payment.
- Reduce administrative burdens and automate many of the administrative tasks involved in RCM.
- Navigate the intricate healthcare landscape with built-in features and capabilities designed for compliance (e.g., HIPAA).
- Ensure that the billing process is both efficient and transparent, as this significantly enhances the patient experience.

Healthcare’s financial pressures continue to grow. Organizations need technology that addresses current revenue challenges while supporting state-of-the-art solutions. Salesforce delivers this combination through detailed tools that optimize today’s complex revenue cycle. It also enables tomorrow’s subscription-based care models for more predictable revenue and customized patient experiences.

